Knee Pain

A Comprehensive Guide On Electrical Stimulation Therapy For Knee Pain
Read More
If you are considering knee surgery for the discomfort and disability caused by your knee pain, you are certainly not alone.
Since the first knee replacement was performed in the late 1960s, knee arthroplasty has become a popular and accessible solution for conditions that cause debilitating joint pain and reduced range of motion.
According to the 2021 American Joint Replacement Registry Annual Report, the number of joint replacement surgeries has increased by 18.3% since 2020. And, between 2012 and 2020, the number of primary knee surgeries performed in the U.S. surged to 1.2 million.
But despite how popular these surgeries are, they are not always the best option for knee pain – nor the only one. By learning more about alternative treatment options, patients can prevent or delay knee arthroplasty and avoid the cascade of consequences, complications, and side effects of invasive surgical procedures.
In this guide, you’ll learn more about the implications of arthroplasty and how non-surgical treatments – such as viscosupplementation and neurofunctional therapies – can help protect your knee health. Let’s get started.
Arthroplasty is a term derived from the Greek words for joint (“arthro”) and molding or grafting (“plastos”). It describes the surgical process that involves reshaping, reconstructing, or replacing one or more components of a joint. Knee arthroplasty is also commonly referred to as “knee replacement surgery”.
Although orthopedic surgical techniques and tools have been developing significantly since the first arthroplasty was performed in 1968, knee replacement surgery is a complex and often invasive procedure that comes with significant side effects.
Today, knee arthroplasty is mostly recommended for end-stage symptomatic conditions that have not responded well to pharmaceutical or physical therapies, such as advanced osteoarthritis that has caused structural damages to bones and soft tissues.
If you are in the process of considering knee replacement surgery to treat your knee pain, you are probably wondering what to expect from this procedure. Learn more about it below.
Before a knee arthroplasty, your surgeon will take you through the necessary steps to prepare you for the procedure, reduce the risk of complications such as periprosthetic joint infections, and ensure that you are fit for knee surgery. These include:
The way knee replacement surgeries are performed may vary depending on what area of the knee is affected. However, in general, your surgeon will start by administering a general or regional anesthetic.
The surgeon will then make an incision in the knee area. The surgeon will insert specialized tools to remove any affected portion of soft and hard tissue (i.e. the cartilage and bones). Then, a metal or plastic implant (prosthesis) will be inserted into position and secured, often using medical cement. Lastly, the surgeon will close the incision and ensure the different parts of the implant can move properly.
Knee replacement surgery can last anywhere between 1 and 3 hours. The type of care and treatment you’ll need after the intervention largely depends on the extent of the surgery.
Generally, you will be moved into the recovery room straight after the procedure, and a team of healthcare professionals will monitor for signs of complications. In some cases, you might be able to go home the same day (outpatient procedures), but some patients spend one night or more in the hospital after their surgery.
Physical therapy usually begins around 48 hours after surgery, and full recovery is usually achieved within 6-12 weeks. In terms of results, knee replacement surgeries can lead to a decrease in knee pain, improved range of motion, and reduced need for pain medications. According to a 2019 study published by the Lancet, 82% of knee surgeries last for up to 25 years.
There are two main types of knee replacement surgeries: total knee arthroplasty and partial knee arthroplasty. Let’s look at these surgeries in more detail below.
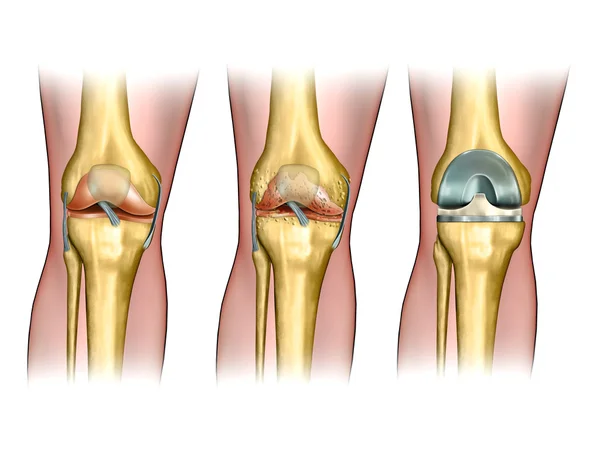
Total knee arthroplasty (TKA) surgery is necessary when the entire knee joint needs to be replaced. This happens if all three components of the knee are affected by osteoarthritis or injury and require surgical intervention.
These are:
Total knee surgery usually resurfaces all three components of the knee. The surgery may also involve replacing or removing the ligaments between the bones (such as the anterior and posterior cruciate ligaments).
A partial knee arthroplasty – also called a unicompartmental knee replacement – is less invasive than a total knee replacement. The aim is to maintain most of the original structure of the knee, and only replace the affected compartment of the knee. This might be the case for patients with knee osteoarthritis, where the arthritis has only affected one compartment in the knee, such as the medial compartment.
Given the impact that a knee replacement can have on a patient’s health and body mechanics, surgery is usually only a last resort after other conservative treatments have been unsuccessful. Surgery is usually only recommended in the case of traumatic injuries and end-stage degenerative diseases, often after other treatment options such as physical therapy and medications have failed.
In particular, knee arthroplasty might be suggested by a healthcare provider to treat the following conditions of the knee:
In most cases, knee replacement surgeries are recommended to ease debilitating or disabling pain, swelling, and stiffness deriving from the conditions above.
Although knee replacement surgeries are generally considered to be highly successful procedures, it is important for patients not to take the decision of undergoing surgery lightly. Even in the best-case scenario, these surgical procedures involve months of rehabilitation and physical therapy before a patient can return to normal activities.
Additionally, healthcare professionals need to inform their patients regarding the risks and complications of knee replacement surgeries, which can also lead to an increased need for revision surgeries. Let’s look at the most common risks of knee arthroplasty below:
Although only around 1% of patients undergoing arthroplasty will develop an infection, this is one of the most common complications of such surgical procedures. Generally, infections are caused by bacteria and affect the wound caused by the surgical incision.
However, in some cases, bacterial infection can affect the periprosthetic joint itself (the area of the joint that has been replaced with plastic and metal parts). Although this can happen at any time after the surgery, it is more likely in the first two years after surgery, which is when up to 70% of infections occur.
You might be at greater risk of developing an infection after surgery if you have immune deficiencies, diabetes, circulatory problems, or if you are obese.
Aseptic loosening is another common surgical complication of knee replacement surgery. This occurs when the prosthesis begins to loosen and fails. This is often caused by improper initial implantation of the periprosthetic joint components, inflammation, or osteolysis (degeneration of the bone tissue attached to the prosthesis).
Aseptic loosening is more likely in patients who had to undergo a revision surgery because they experienced periprosthetic infection after their primary knee arthroplasty. In particular, among these patients, the prevalence of prosthetic loosening is as high as 22% after 7 years of the surgery.
Metallosis is an uncommon complication of joint replacement surgery, but it is more likely to happen in arthroplasties of the knee, hip, or other high-wear joints. This condition causes an abnormal buildup of metallic particles and debris around the periprosthetic implant and surrounding joints.
A BMJ case study reported that around 7 out of 30 patients who underwent a TKA involving metal-backed patellar components developed metallosis.
Dislocation of the periprosthetic knee can happen in a similar way to natural knee dislocations, including trauma and overextension. However, there are additional factors that increase the risk of dislocation.
These factors include implant malpositioning, inappropriate selection of the implant, deformity, and hardware malfunction, such as the breakdown of the polyethylene (plastic) lining between the prosthetic parts.
TKA dislocations account for 0.02-0.2% of orthopedic injuries among all patients, and 0.15-0.5% of injuries in people with arthroplasty.
Beyond dislocation, less severe instability issues in TKA patients can happen due to mechanical malfunction affecting the periprosthetic knee.
As the population continues to age and the number of knee replacement surgeries performed each year increases, the prevalence of periprosthetic fractures is also rising. This complication can happen any time after the surgery and involves a fracture in one or more bones around the area where the prosthesis was implanted.
Periprosthetic fractures almost always require surgery. Currently, this condition is estimated to affect between 0.3% and 5.5% of TKA patients.
The patellofemoral joint is located in front of the knee. Because of this joint’s location, it is connected to some of the components of the knee joint including the patella (kneecap). After a total knee arthroplasty, it is not uncommon for patients to experience complications such as patellofemoral pain.
A 1995 study shows that, at the time, patellofemoral complications were present in 12.8% of patients who had undergone TKA. Additionally, the same study mentions that the prevalence of this complication is higher among older and overweight patients.
For those battling end-stage symptomatic conditions of the knee – including osteoarthritis – surgery might seem like the only and inevitable option. And, for some individuals, it is.
However, for those patients looking to prevent or delay knee replacement surgeries, it is important to learn about the alternative treatment options that can help, such as the ones offered by Relatyv.
At Relatyv, our team of healthcare professionals and researchers have developed a customized treatment protocol that can help ease knee pain, support tissue regeneration, and lower the risk of surgery. These treatments are non-surgical, non-pharmaceutical, and are backed by science.
Below are the three pillars of the treatment protocol for knee pain offered at Relatyv:
For patients with knee pain that has not responded to exercise and physical therapy, it is important to look for non-opioid, long-term solutions such as TriVisc.
TriVisc injections work by delivering hyaluronic acid (HA) into the joint area. Here, the HA will form a gel-like substance called hyaluronate. This substance is naturally produced by the body and helps regulate how the joint tissue responds to injury. It also plays a vital role in keeping the joints healthy, lubricated, and safe from shock and friction.
Over time, the supply of HA in the body declines, often due to age and factors like smoking. Thanks to TriVisc injections, Relatyv can help replenish the supply of HA in the joint, thus easing discomfort, decreasing inflammation (such as in the case of arthritis and osteoarthritis), keeping the joint lubricated, and providing long-lasting comfort.
Visco, short for viscosupplementation, is a treatment that involves injecting hyaluronic acid into diarthrodial joints. Diarthrodial joints – which are freely movable joints such as the knee – are joints that rely on two components to keep motions smooth and lubricated. These two components are:
When this system wears down over time, the joint’s components and the surrounding bones might be exposed to damage caused by shock and friction. Viscosupplementation therapies aim to restore the synovial fluid with hyaluronic acid.
This can have a powerful lubricative and analgesic effect, reducing inflammation, easing swelling, and relieving joint pain. According to 2015 studies, viscosupplementation can delay the need for total replacement surgery by 3 years or more.
The proprietary Neurofunctional Pain Management protocol designed by Relatyv helps ease pain naturally and support the regeneration of damaged tissue when combined with the therapies above.
At Relatyv, we use hydration therapies and high-pulse electrical stimulation (electroanalgesia) to stimulate the production of endorphins, depolarize pain neurons, and deliver long-lasting pain relief. What’s more, thanks to Neurassage – our patented massage therapy – and lifestyle counseling, we are able to help patients regain control of their lives and ease pain without opioids or surgery.
At Relatyv, our goal is to help patients do much more than simply reduce their knee pain. We aim to help individuals magnify their lives, enjoy a lifestyle free of medications, and delay or prevent the need for surgery.