Mild cramps and minor discomfort are a normal part of certain phases of the menstrual cycle. But up to a third of women in their reproductive age experience excruciatingly painful periods, accompanied by intense menstrual cramps that start days before the menstruation and continue long after their period ends. These painful sensations aren’t just debilitating – they can also be life-limiting, get in the way of your daily life, and affect your ability to work or take part in social activities.
Painful periods – a condition known as dysmenorrhea – are certainly not normal, and they can be a symptom of a more serious underlying condition. With an accurate diagnosis provided by our specialists and a tailored Neuragenex Neurofunctional Pain Management program, you can identify and address the root causes of your condition without medications or surgery. Learn more below.
How Do Menstrual Periods Cause Pain?
The menstrual cycle is a complex process that engages several glands, hormones, and organs. It is composed of four main phases:
- Follicular: During the follicular phase, which starts on the first day of your cycle and lasts for up to 14 days, the body releases hormones that stimulate the production of follicles on the internal surface of an ovary. Only one of these follicles will then mature into an egg.
- Ovulation: During ovulation, a mature egg transfers from the ovary to the uterus via the Fallopian tube. Ovulation may last anywhere between 16 and 32 hours, and it represents the time during which a woman is most fertile.
- Luteal: After ovulation, the interior lining of the uterus (endometrium) begins to grow, thicken, and swell in preparation for pregnancy. If you are pregnant, the endometrium will support the growth of the fetus and safeguard the egg from microbial invasions.
- Menstruation: If the egg is not fertilized and you are not pregnant, the body expels the unneeded endometrium through menstruation.
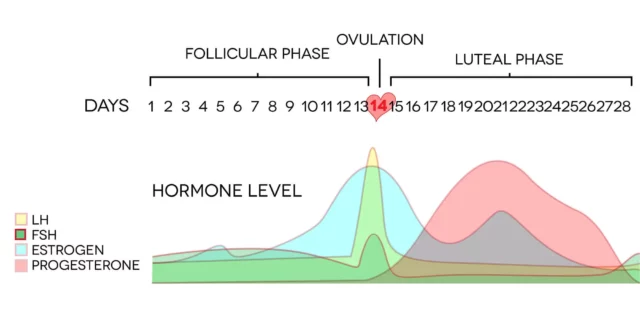
During the menstruation phase – or your period – the body produces high levels of a hormone called prostaglandin, which is responsible for triggering the muscle contractions needed to expel the lining of the uterus. However, these contractions can cause pain, and high levels of prostaglandin may increase inflammation in the uterus and surrounding organs.
Painful menstrual cramps may also be accompanied by other symptoms like constipation, diarrhea, and nausea.
Types Of Period Pain
There are two types of dysmenorrhea:
- Primary Dysmenorrhea: If you have primary dysmenorrhea, painful menstrual cramps are, in themselves, the condition. They are not caused by another underlying disorder, start just after your menarche (first menstruation), and accompany every menstrual cycle you experience. The pain from primary dysmenorrhea can range from mild to severe, change over time, and disappear after 2-3 years. This is the most common form of dysmenorrhea.
- Secondary Dysmenorrhea: Secondary dysmenorrhea refers to painful periods caused by another, underlying medical condition. This type of dysmenorrhea is usually more intense and lasts longer than normal menstrual cramps, and it can develop at any point in a woman’s reproductive life.
Secondary dysmenorrhea accounts for less than 8% of cases of painful menstrual cramps, and it is most commonly caused by endometriosis.
Pain Thresholds During Menstruation
Several studies have been conducted to determine how the pain threshold changes across the different phases of the menstrual cycle.
Research published in 2003 shows that pain sensitivity levels were significantly higher in the menstrual and premenstrual phases of the cycle, also due to the rise in prostaglandin. Those who experienced intense pain were also more likely to have a passive coping style and catastrophizing thoughts. On the other hand, studies have shown that the highest pain tolerance occurred during the follicular phase.
Additionally, given that sex hormones such as estrogen influence how the brain processes pain signals, the hormonal fluctuations that occur during the menstrual cycle may worsen the painful sensations deriving from other conditions, including migraine.
Conditions Associated With Extremely Painful Periods
If you have recently developed extremely painful periods, you may have secondary dysmenorrhea. This means that simply treating the pain, cramping, and discomfort you experience during the menstrual cycle isn’t enough to regain your pelvic health. Even worse, when left unaddressed, certain conditions that cause painful menstrual cramps can lead to infertility.
Identifying the root cause of your painful periods is the first step to obtaining an accurate diagnosis and selecting an efficient line of treatment. Let’s look at the most common causes of dysmenorrhea below.
Endometriosis
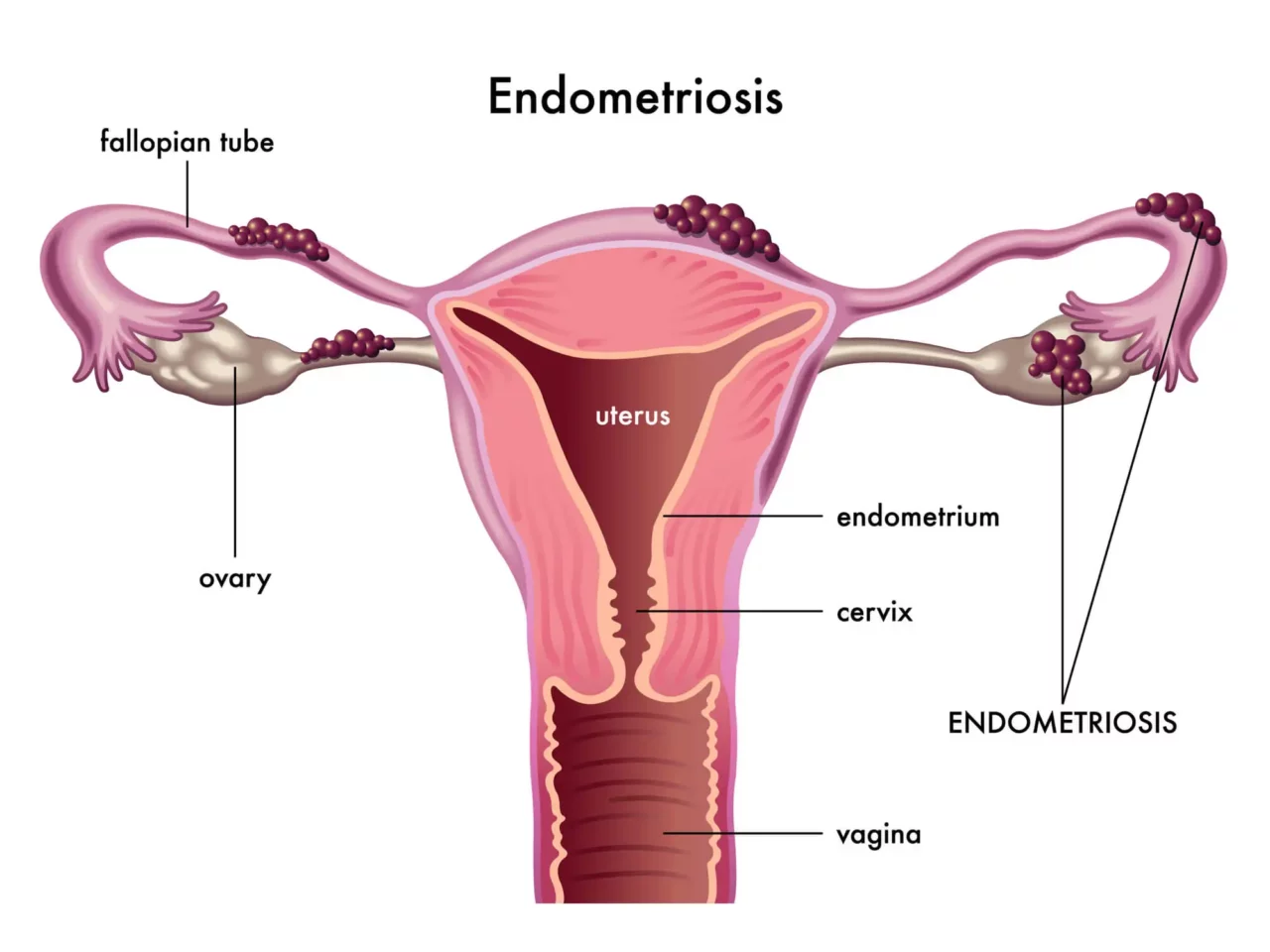
Endometriosis occurs when the endometrial growths (lining of the uterus) that thicken and swell during the luteal phase begin to grow outside of the uterus, usually on the ovaries, fallopian tubes, pelvic cavity, cervix, vagina, and bladder.
During the different phases of the cycle, this abnormal endometrial tissue behaves just like the endometrium inside the uterus: it is hormone-dependent and grows and thickens during the luteal phase. However, unlike the endometrium, the endometrial implants outside of the uterus are unable to leave the body during menstruation.
This leads to an accumulation of endometrial tissue outside the uterus that continues to proliferate, swell, and thicken with each menstrual cycle. Over time, this inflamed tissue can lead to scarring, cysts, adhesions (binding between reproductive organs), and infertility.
Endometriosis is the most common cause of secondary dysmenorrhea. This condition affects over 6.5 million women in the US alone and causes patients to lose an average of 6 hours a week of productivity.
Endometriosis is also associated with other life-limiting symptoms, including dyspareunia (pain with sexual intercourse), painful bowel movements, excessive bleeding, and gastrointestinal issues. Despite how common and debilitating endometriosis is, 90% of people with this condition report feeling dismissed or disbelieved by their doctors or loved ones.
Premenstrual Syndrome (PMS)
Around 90% of women in their reproductive age experience premenstrual syndrome to some extent. This condition is characterized by a range of symptoms, including emotional tension, anxiety, depressed mood, changes in appetite, poor concentration, and a change in libido. PMS also causes joint or muscle pain, headaches, bloating, acne flare-ups, fluid retention, and constipation or diarrhea.
PMS usually occurs 1-2 weeks before the menstruation begins, and the symptoms ease down when your period begins. Although the causes of Premenstrual Syndrome are not always clear, it is believed that it may arise due to hormone fluctuations and changes in brain chemicals.
Fibroids
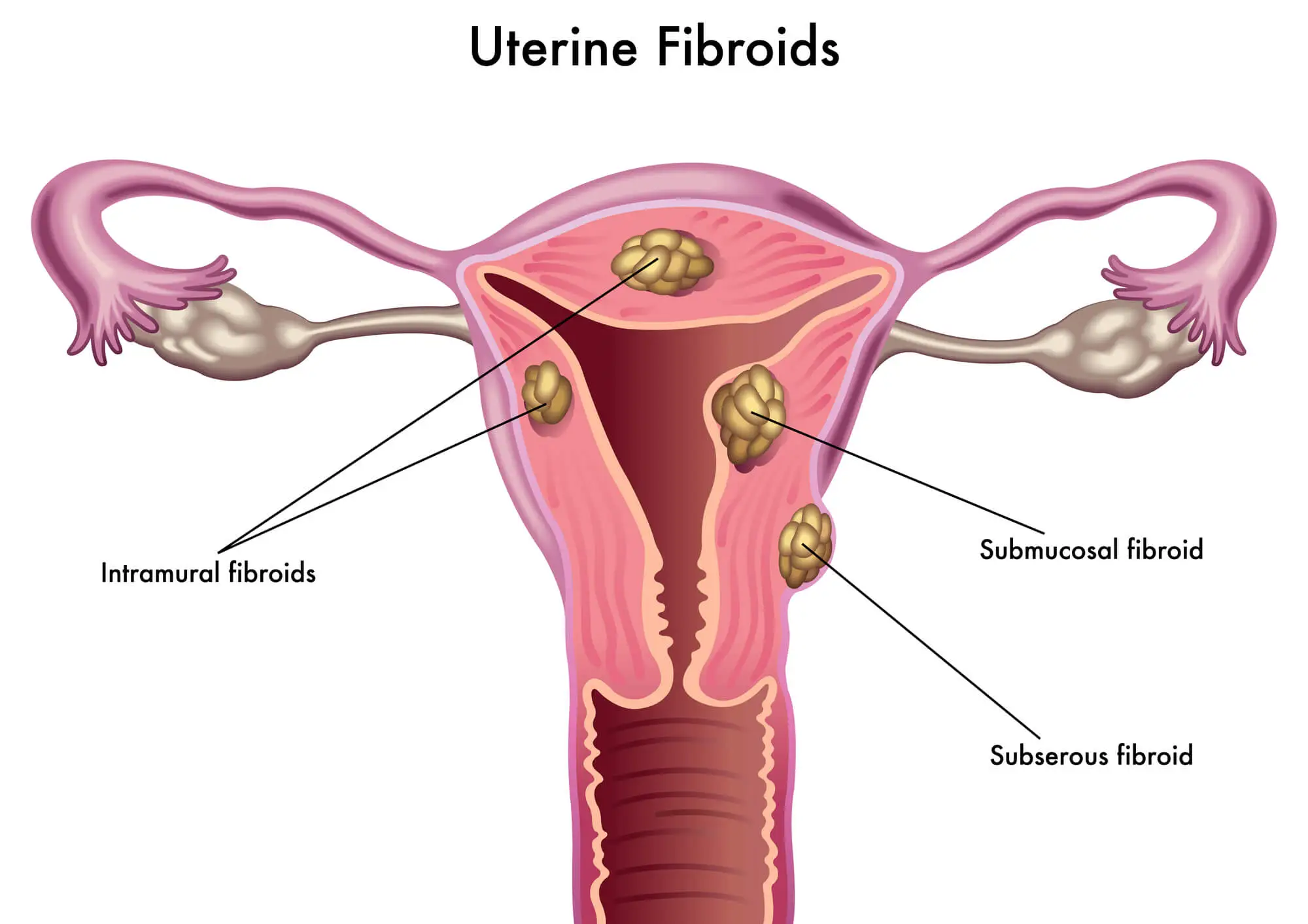
Fibroids (uterine fibroids) – also known as myoma – are non-cancerous tumors that develop from muscle tissues within the womb and grow in or around the uterus, the cervix, and in the fallopian tubes.
Fibroids may continue to grow over time and become very large. This can lead to a cascade of severe consequences, including secondary dysmenorrhea and painful cramping. Other symptoms that you may have fibroids in your uterus include having a bulging belly (as if you were pregnant), pressure on pelvic organs, frequent urination, and difficult bowel movements.
Although, sometimes, fibroids don’t cause symptoms, they should not be left unaddressed. Doing so can lead to problems during pregnancy and childbirth.
Pelvic Inflammatory Disease
Pelvic Inflammatory Disease (PID) is an inflammatory condition that affects the reproductive organs of a woman, including the uterus, fallopian tubes, and ovaries. PID is sexually transmitted and often develops as a complication of other STDs, such as chlamydia. 2.5 million women in the US alone have been diagnosed with this condition during their lifetime.
Besides dysmenorrhea, PID can cause pelvic pain, pain during sex, painful urination, bleeding between periods, heavy and painful periods, and abnormal vaginal discharge. Although this condition can be easily treated with a course of antibiotics, it is important not to let PID go unaddressed, as doing so can lead to infertility.
Adenomyosis
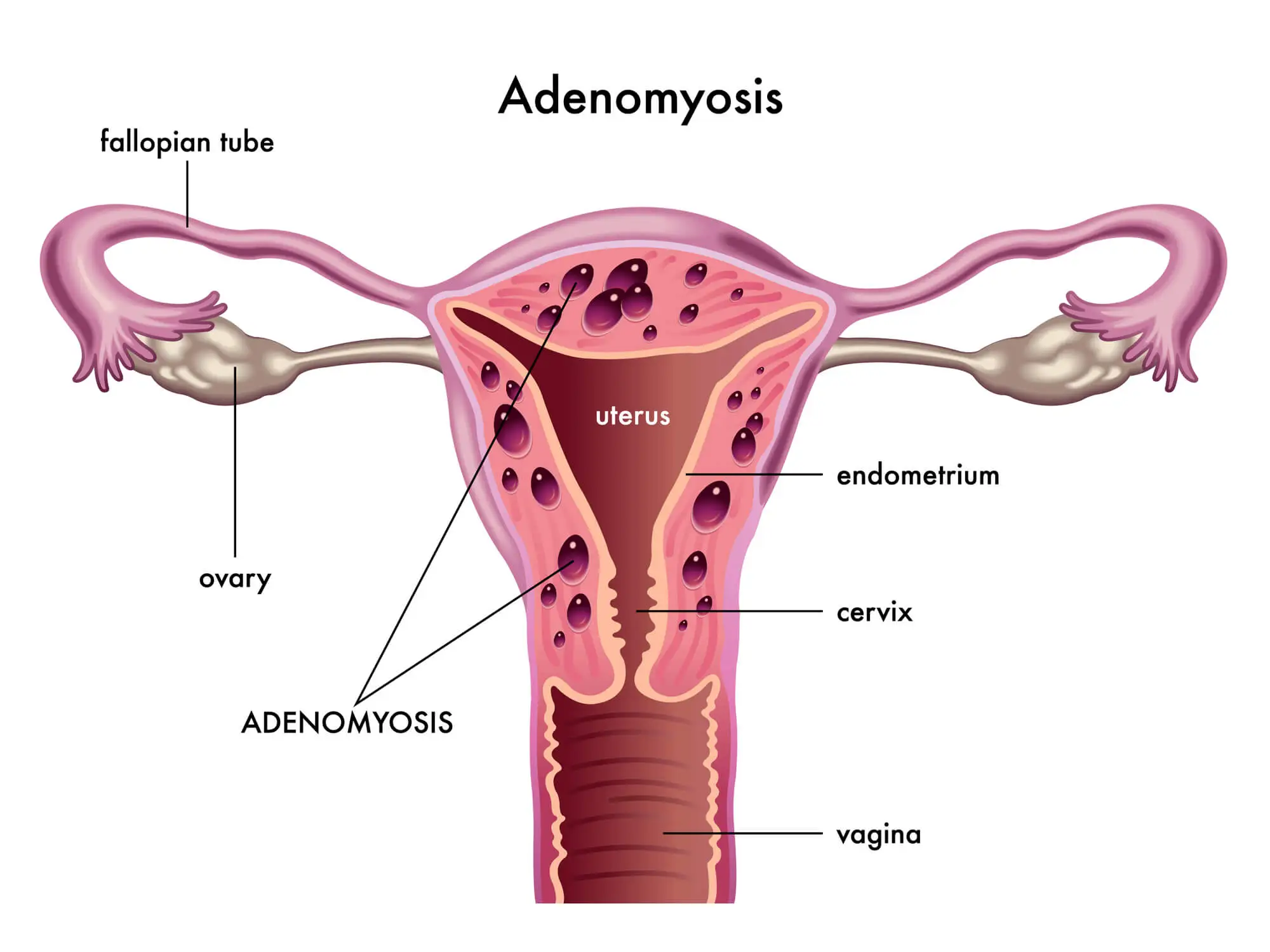
Adenomyosis is a condition that occurs when the endometrium (the lining of the uterus) grows into the muscular wall of the uterus. Similarly to endometriosis, these endometrial implants grow and thicken with each menstrual cycle but are unable to leave the body during menstruation. This leads to inflammation, pain, pressure, and an enlarged uterus. If you have adenomyosis, you may also experience dysmenorrhea and excessive bleeding,
Although adenomyosis can affect 1 in 10 women of reproductive age, the extent and severity of this condition varies from one person to another.
Cervical Stenosis
Cervical stenosis is a condition that causes the narrowing or closing of the passageway located in the lower part of the uterus, known as the cervix. This passageway is used by the menstrual blood to leave the body during menstruation. If the cervix is too small, it can slow down the menstrual flow, which increases pressure, pain, and inflammation inside the uterus during menstruation.
This condition also leads to menstrual abnormalities, infertility, hematometra (the accumulation of blood in the uterus), and, if the menstrual blood flows back into the fallopian tubes and ovaries, endometriosis.
Conditions We Treat With Neuragenex Neurofunctional Pain Management

Endometriosis Pain Treatment
Endometriosis is a condition that can cause severe and chronic pelvic pain, heavy menstrual bleeding, and other uncomfortable symptoms. Pain caused by endometriosis can be debilitating and may prevent you from living a full, active life. Fortunately, we offer...
Risk Factors For Painful Menstrual Periods
Painful menstrual periods can affect any person who menstruates at any point in their reproductive age. However, as outlined by a 2021 study, certain factors may increase your risk of suffering from this condition, including the following:
- Being under 20 years of age: Primary dysmenorrhea tends to decrease in intensity over time, and it disappears with menopause. If you suffer from this condition, painful symptoms associated with your period will begin to appear within a few months or years of your menarche and improve significantly after the age of 40, even if you have never given birth to a child.
- Family history of painful periods: According to a 2014 study, having a family history of dysmenorrhea significantly increases the risk of developing this condition.
- Smoking: Smoking narrows the blood vessels, inhibits the supply of oxygen and nutrients to the reproductive organs, and increases inflammation. Additionally, smoking can influence hormonal activity, have toxic effects on the ovaries, and increase the risk of experiencing severe cramps that last two days or longer.
- Heavy bleeding with periods: If you have menorrhagia (heavy or prolonged menstrual bleeding), you are more likely to suffer from painful cramps because of the excessive cramping and prostaglandin secretion involved with menstruation. This condition may be caused by a range of conditions, including hormonal imbalances, dysfunction of the ovaries, and adenomyosis.
- Irregular periods: Irregular periods can put you at greater risk of suffering from dysmenorrhea. Periods that are both irregular and painful may be a symptom of another underlying condition, including endometriosis, polycystic ovarian syndrome (PCOS), or fibroids.
- Not experiencing pregnancy: Being nullipara, or never having given birth to a child, can increase your risk of experiencing painful periods. However, the pain should ease down after the age of 40.
- Reaching puberty before age 11: An early menarche may be associated with more painful periods, as well as conditions that cause secondary dysmenorrhea, such as endometriosis and fibrosis.
Other risk factors for painful periods include drinking alcohol, several attempts to lose weight, a history of depression or anxiety, and disruption in your social or personal life.
When To Seek Medical Attention For Menstrual Period Pain
No matter when you develop painful periods, dysmenorrhea can be a life-limiting condition that impacts all aspects of your life. For example, among adolescents, dysmenorrhea is a leading cause of school absenteeism, while adult women with painful menstrual cramps may be unable to work, participate in sports, or enjoy their hobbies.
But what’s even more concerning is the fact that painful periods may be caused by an underlying condition that, if left treated, can lead to severe complications such as infertility. Because of this, knowing when to see a doctor for your painful periods is vital. Here are the telltale signs that should not go unnoticed:
- Debilitating pain during periods: Whether you have primary or secondary dysmenorrhea, if the pain and discomfort you experience each month get in the way of your daily life, you should seek medical attention immediately.
- Chronic pain outside of menstruation: Chronic pain outside of menstruation or cramps that start several days before your periods and continue long after are a sign that you may be dealing with an underlying condition like endometriosis. A specialized doctor can help you obtain an accurate diagnosis.
- Painful sexual intercourse: Dyspareunia, or painful sex, is a condition that affects up to 18% of women. It can be caused by a wide range of conditions, including uterine fibroids, pelvic inflammatory disease, endometriosis, cystitis, irritable bowel syndrome, and ovarian cysts. If you are experiencing this symptom, a doctor can help you identify and treat the root cause of your pain.
- Ovarian cysts: Ovarian cysts are sacs filled with fluids that develop inside an ovary. This is a serious condition that causes symptoms such as swelling, bloating, pain in the pelvis, and painful sex.
- Infertility: Unexplained infertility may be caused by several conditions that are also the source of painful periods, including endometriosis, polycystic ovary syndrome (PCOS), and Pelvic Inflammatory Diseases (PID).
- Fever: When your body produces prostaglandins before your period, you may experience what’s known as “Period Flu”, or low-grade fever. However, if your fever is rising, or accompanied by excessive bleeding, prolonged periods, and severe cramps, you should immediately visit a doctor.
- No response to pain medication or home remedies: Primary dysmenorrhea usually responds to anti-inflammatory non-steroidal drugs and home remedies such as warm compresses. If your pain continues after your period or intensified over time, you may be dealing with another underlying condition that requires medical attention.
Diagnosing Heavy Painful Periods
As we have seen above, one of the leading causes of secondary dysmenorrhea is endometriosis. To provide you with an accurate diagnosis and a comprehensive clinical picture, your doctor may carry out the tests necessary to understand whether painful menstruation may be caused by endometriosis or another condition. These tests include:
- Complete Blood Count (CBC) Test: A CBC with differential is used to determine the presence or absence of infections or other abnormalities. This type of test is recommended to all women – especially those aged 35 and above – even if they don’t experience significant problems.
- Lab Cultures Lab cultures are used to determine the presence or absence of sexually transmitted infections and diseases, such as chlamydia, that may be the source of painful periods.
- Laparoscopy: Laparoscopy is a surgical and diagnostic procedure that involves inserting a laparoscope (a thin viewing instrument) through small incisions performed around the pelvis area. The laparoscope can be guided to view the uterus, collect samples of tissues for testing, and remove abnormal growths that may be causing pain.
- Pelvic Ultrasound: High-frequency sound waves can be used to obtain clear images of the inner pelvic area. This helps doctors determine the presence and extent of endometrial implants that may be causing pain.
Depending on your symptoms, a healthcare provider may also use imaging tests (i.e.: MRI scans) to obtain a clear view of the presence, location, and severity of endometrial implants.
Neuragenex NFPM Protocol To Manage Painful Menstrual Period
Patients dealing with dysmenorrhea and endometriosis are often disbelieved, dismissed, or left to deal with the stigma that still surrounds menstruation. However, the pain deriving from these conditions is real and debilitating.
Educating yourself about the causes, symptoms, and prognosis for painful periods and endometriosis can help you look beyond just taking medications daily to manage your pain.
With the right knowledge and guidance, you can explore the non-invasive, non-pharmaceutical, and non-chiropractic approach of Neuragenex Neurofunctional Pain Management. Below, we’ll look at the three main columns of this whole-person approach designed around your needs.

Electroanalgesia
Electroanalgesia is a pain management technique that uses high-pulse electrical current to ease pain, boost blood circulation, improve mobility, and induce...
IV Therapy
IV nutritional therapy, or intravenous therapy, involves administering vital nutrients directly to the bloodstream through an IV. This type of treatment bypasses the digestive system, allowing for maximum absorption and utilization of nutrients by the...
Lifestyle Counseling
Lifestyle counseling is an approach to managing chronic pain that involves identifying, assessing, and modifying lifestyle factors contributing to an individual's pain. For example, lifestyle factors such as nutrition, physical activity, stress, sleep quality...
Say Goodbye To Painful Menstrual Periods
If you have been dealing with painful menstrual cycles, the chances are that each month, you rely on medications to be able to go to work, meet your friends, or simply keep up with your household responsibilities. But, if you are tired of living a life reliant on medications, we can help.
Thanks to Neuragenex Neurofunctional Pain Management, we can provide patients battling painful periods and endometriosis with a whole-person approach to managing pain without medications or surgery.
There’s a new way of treating period pain. Find out more about how we treat menstrual period pain related to endometriosis.




