Everyone experiences paresthesia at least once in their lives. Think, for example, of when you’ve been sitting cross-legged for too long and you have the sensation that your limb has “fallen asleep.” Or it can happen while you are asleep, often because your arm or hand has gone numb from being twisted under your head.
This “pins and needles” sensation occurs when certain nerves are pressured and are unable to send signals to the brain relating to movement or sensation. Some forms of paresthesia are temporary and benign – and can be resolved by shifting your body’s position.
However, if this symptom is recurring, chronic, or getting worse over time, you should seek an accurate diagnosis: paresthesia can be a telltale sign of a severe condition affecting your musculoskeletal or nervous system (e.g. sciatica, neuropathy, multiple sclerosis).
In this guide, we’ll look at what paresthesia is and what causes pins and needles sensations. We’ll also look at how the whole-person approach –Neuragenex Neurofunctional Pain Management – can help you address the systemic inflammation and chronic pain at the root of your condition without medications or surgery. Let’s get started.
Recognizing The Prickly Sensation
Pins and needles is a condition medically known as paresthesia. This refers to burning or prickling sensations that are commonly felt in the limbs but can spread to any area of the body.
The most common culprit of paresthesia is sustained pressure on a nerve. This can occur when you are lying in a certain position for too long or sitting with your legs crooked under your body.
Depending on what nerve is pressured, you may experience pins and needles in the following locations:
- Hands
- Feet
- Arms
- Legs
If these sensations are caused by temporary pressure on a nerve, changing position will restore the normal function of your limbs in no time. However, in some cases, recurring paresthesia or numbness that spreads from your limbs across the body can indicate a severe underlying condition, including damage to the nerves in the central or peripheral nervous systems.
Other Symptoms Associated With Pins And Needles
Paresthesia usually manifests itself with pins and needles sensations. However, you may also experience a wide range of symptoms in the areas affected, including:
- Burning
- Itching
- “Skin crawling”
- Numbness
- Tingling
- Pain (sometimes described as dull)
Paresthesia usually happens without warning and can develop in a matter of minutes when a nerve is compressed. If it derives from a pinched, damaged, or irritated nerve, these sensations can also continue spreading over time.
In particular, when it is a symptom of nerve damage (neuropathy), paresthesia tends to occur first in the fingers and toes, only to progress towards the hands, feet, arms, and legs. This occurs due to a phenomenon known as “axonal degeneration” or “dying back.” This phenomenon dictates that the first nerves to be affected by damage are the ones further from the spinal cord and the brain (i.e. those serving the limbs) to protect more important nerves that support the function of vital organs.
Possible Underlying Conditions
Although pins and needles sensations may occur without an apparent reason, recurring episodes of paresthesia should not go unaddressed.
Whilst this condition is often temporary and can be resolved in a matter of minutes, when it occurs repeatedly or gets worse over time, it may indicate underlying problems with your peripheral or central nervous systems.
Peripheral Neuropathy
One of the most common causes of paresthesia is peripheral neuropathy. Peripheral neuropathy is a condition that leads to progressive nerve damage, thus interfering with the normal transmission of signals from the nerves around your body (peripheral nerves) to the central nervous system (the brain and the spinal cord). When this transmission is interrupted, you are likely to experience pain, numbness, and pins and needles. It is estimated that nearly 90% of people with neuropathy have painful symptoms that include tingling, burning, and prickling sensations.
Nerve damage can occur due to a range of reasons, including:
- Diabetes (up to 50% of people with diabetes mellitus report neuropathy in some form)
- Exposure to toxins
- Vitamin deficiencies (especially vitamin B12)
- Lifestyle factors (e.g. aging, alcohol consumption, and smoking)
- Certain medications (e.g. chemotherapy)
- Tumors that press on or damage nerves
- Unknown causes (up to 30% of cases of neuropathy are idiopathic)
Besides neuropathy, there are other conditions that can cause you to experience paresthesia or pins and needles sensations. Let’s look at these in more detail below.
Nerve Compression
One of the most common causes of pins and needles is, simply, the sustained compression of a nerve, also known as a “pinched nerve.” Sometimes, such nerve compression occurs due to an awkward position of parts of your body, commonly the limbs. This may be the case if you fall asleep with your arm under your head or sit in a cross-legged position for a while. It may also occur when bumping your elbow against a hard surface or corner.
Recurring episodes of paresthesia may be a sign that there’s something else compressing one or more nerves. These include:
- Abnormal tissue growth next to the nerves, such as tumors
- Swelling of tissues around the nerves
- The narrowing of the canal that houses the nerves, such as in the case of peroneal nerve dysfunction, carpal tunnel syndrome or spinal stenosis
- Abnormal overgrowth of bone (bone spurs)
- Improper mechanics, such as poor posture
- An old or new injury that has caused another component of the body to slip out of place and press on a nearby nerve
- Medical conditions that cause changes in the body, such as a herniated disc pressing on a nearby nerve
- Genetic and hereditary factors, such as having a carpal tunnel that’s too small
An accurate analysis of your symptoms and medical history is necessary to determine what’s causing your nerve compression and pinpoint the best line of treatment for your needs.
Poor Blood Circulation
Poor blood circulation prevents essential oxygen and nutrients from reaching certain parts of the body, which can lead to a wide range of symptoms, including pins and needles. There can be several reasons for reduced blood supply in the hands, feet, or limbs, some more severe than others. These include:
- Lying or sitting awkwardly: The weight of your body can press on blood vessels, which is a common reason for feeling like your limbs have fallen asleep.
- Atherosclerosis: This condition occurs when plaque buildup in blood vessels such as arteries prevents the blood from flowing as it normally should. It can cause sudden numbness and tingling sensations.
- Blood clot: A blood clot can partially or completely block blood flow. This condition can cause numbness, pain, and pins and needles, and, in severe cases, it can lead to a heart attack or stroke.
- Diabetes: Uncontrolled spikes and drops in blood sugar levels can, over time, damage blood vessels, thus interrupting the normal flow of blood.
- Risk factors: Some risk factors, such as smoking tobacco products and being obese, can affect the health of blood vessels and lead to poor circulation.
Diabetes, especially if undiagnosed or uncontrolled, can impair blood flow to nerve endings. This can lead to nerve damage and cause peripheral neuropathy (nerve pain), a condition commonly associated with paresthesia.
Multiple Sclerosis
Multiple sclerosis (MS) is a degenerative, lifelong condition that affects the central nervous system (the brain and the spinal cord). If you have MS, your immune system mistakenly attacks the protective sheath that covers nerve fibers, called myelin.
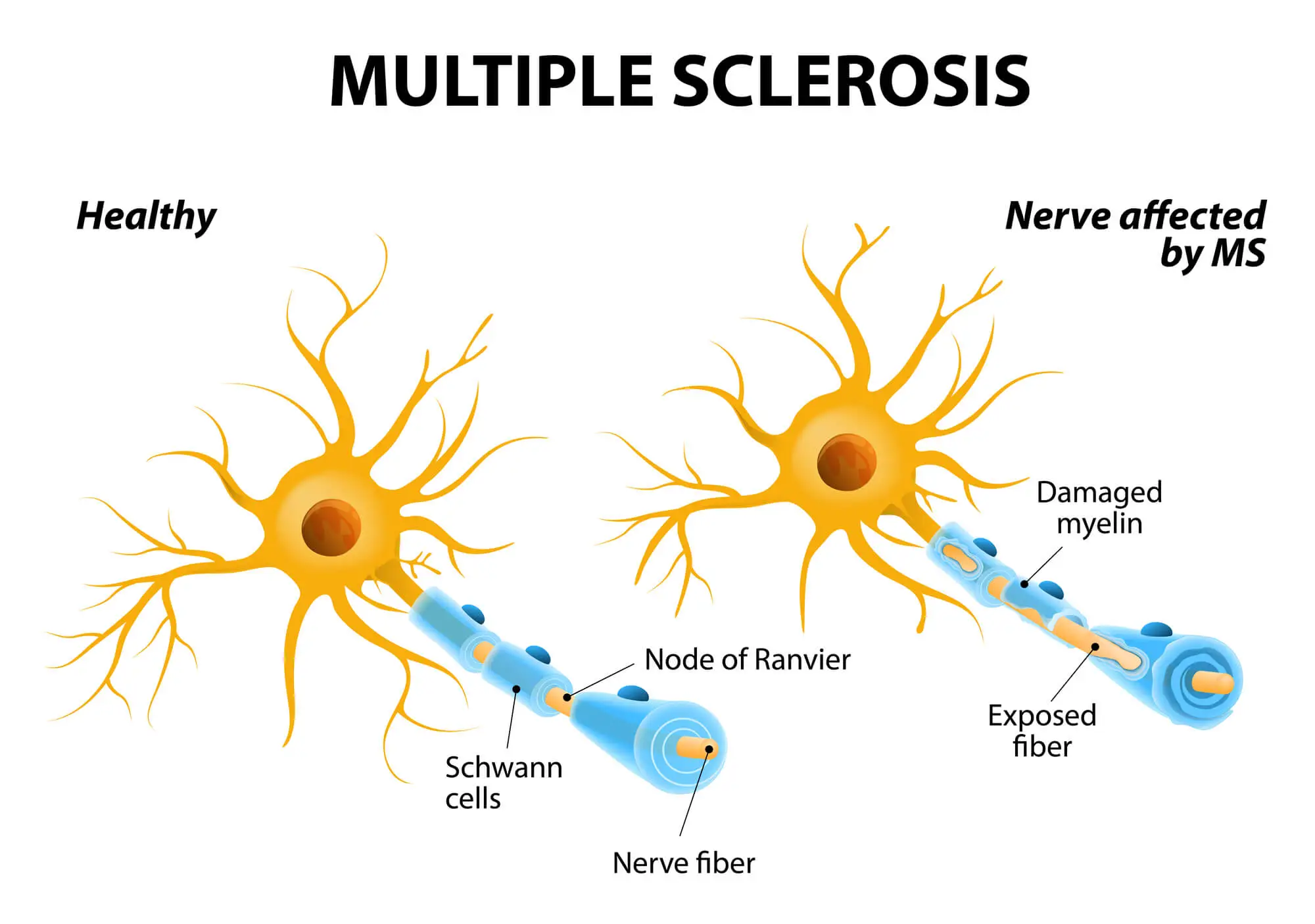
Nerve damage may begin in the hands and feet but tends to progress to other nerves across the body, eventually leading to various degrees of disability. Pins and needles sensations, alongside numbness, tingling, and pain, are some of the early symptoms of MS.
Fibromyalgia
Fibromyalgia is a chronic disorder that causes widespread musculoskeletal pain across the body. The pain caused by fibromyalgia is often described as aching, burning, or throbbing, and it is accompanied by a wide range of symptoms, including paresthesia, mood issues, fatigue, memory problems, and poor sleep quality.
In people with fibromyalgia, painful sensations are amplified due to dysfunction in the way the central nervous system processes painful and non-painful stimuli. It is estimated that today, around 4 million people in the US – or 2% of the adult population – have fibromyalgia in some form.
Sciatica
Sciatica is one of the most common reasons for pins and needles sensations, numbness, and tingling, especially when they occur in the buttocks, hips, legs, feet, and toe areas. Sciatica occurs when the sciatic nerve is pinched, irritated, inflamed, or damaged.
There are two sciatic nerves in your body, one on each side, running from the lower back to the feet. These nerves are among the largest and longest in the body, and they are responsible for transmitting signals relating to touch, temperature, pain, vibration, and movement between the brain and the lower part of the body.
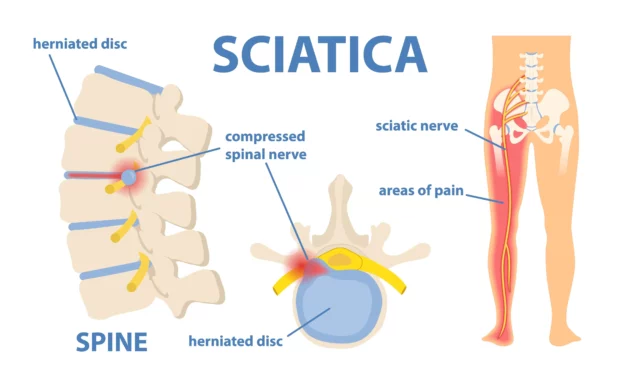
There are several conditions that cause a sciatic nerve to become compressed or irritated, including:
- Spinal stenosis
- Old and new injuries (e.g. fractures or dislocations)
- Herniated or bulging discs
- Poor posture
- Inactivity and prolonged sitting
- Weak core and back muscles
- Occupation, especially if it involves repetitive or forceful movements of the spine
- Risk factors such as aging and obesity
- Medical conditions such as diabetes
Around 40% of people will experience at least one episode of sciatica, and this condition tends to resolve on its own within three to 12 weeks.
Nonetheless, if your symptoms are not going away or getting worse, it is important to seek an adequate line of treatment that does not involve medications or surgery. This is because sciatica-like pain can conceal more severe underlying diseases, which may derive from systemic inflammation. Tackling this root cause is the first step to regain your musculoskeletal health.
Raynaud’s Disease
Raynaud’s disease, also called Raynaud’s phenomenon, occurs in around 3-5% of the population. In people with this disorder, the body triggers an abnormal response to cold or stress, causing spasms in small blood vessels located in certain areas of the body (usually the hands and feet). These abnormal spasms (known as vasospasms) reduce blood circulation, which can lead to a range of symptoms, including paresthesia, numbness, tingling sensations, pain, and skin color changes.
How Are Pins And Needles Sensation Connected To Nerves?
To understand why you experience pins and needles in response to dysfunction with the nervous system, it is important to clarify the role that nerves play in carrying sensations. Here’s a simplified overview:
The nervous system is subdivided into two main parts:
- The central nervous system: The nerves located within the brain and spinal cord
- The peripheral nervous system: The nerves located across the body, outside of the brain and spinal cord
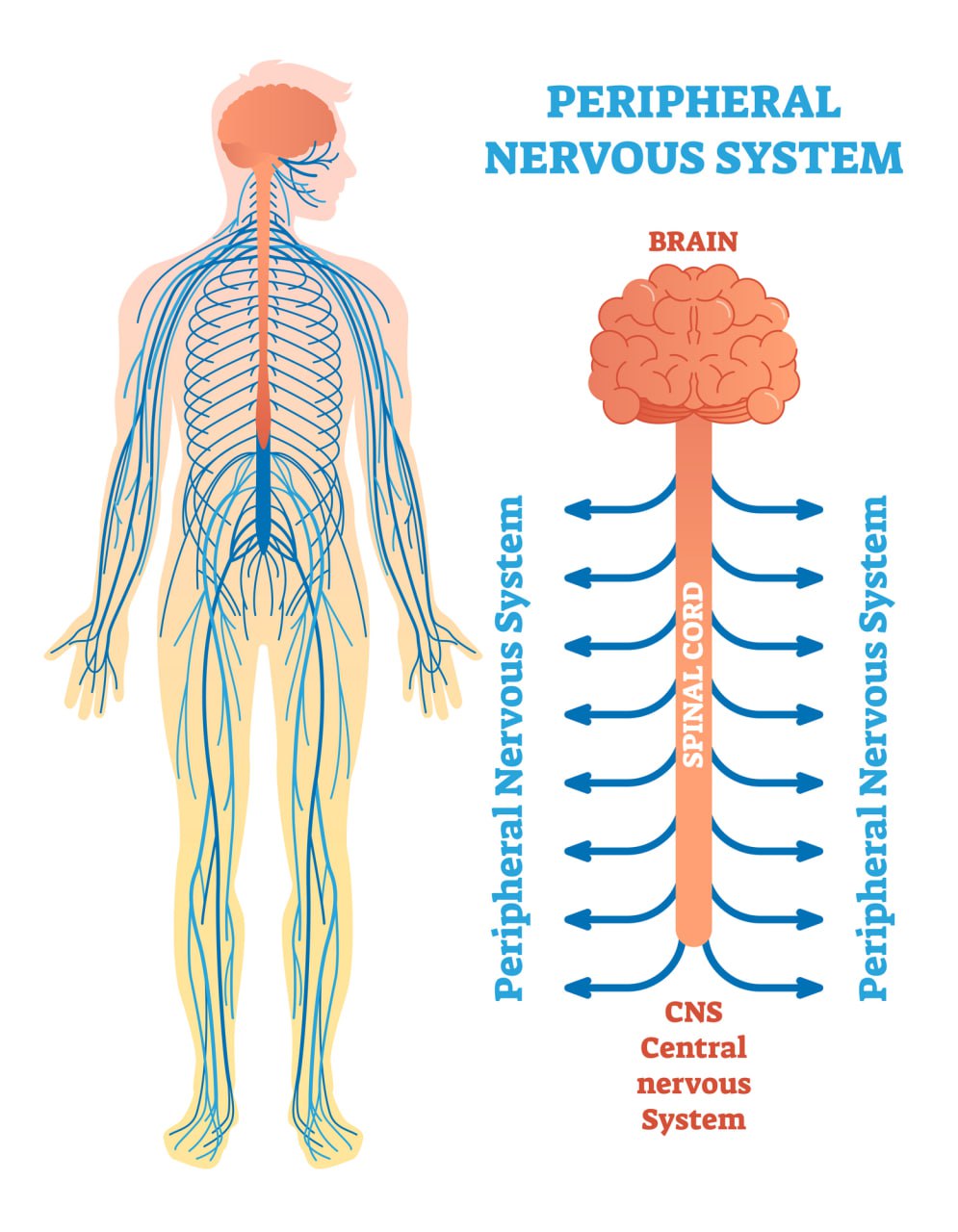
The nerves in the peripheral nervous system are responsible for carrying signals from the different areas of the body to the brain, where they will be processed. These signals can relate to:
- Sensations: These are carried by sensory nerves and involve all of those signals relating to touch, pain, vibration, and temperature.
- Movement: These are carried by motor nerves and include all of those signals relating to muscle movement, coordination, and gland function.
- Autonomic signals: The autonomic nerves are responsible for regulating functions we don’t have direct control over, such as heartbeat, respiration, digestion, and blood pressure.
When the nerves responsible for carrying motor and sensory signals are compressed, damaged, or inflamed, they work at a suboptimal level, preventing signals from reaching the brain. This translates into a sensation of numbness and altered response to stimuli (e.g. being unable to feel temperature and touch).
In severe cases, such as if you have MS or specific forms of neuropathy, the autonomic nerves can be affected too, causing sexual dysfunction, irregular heartbeat, digestive problems, and loss of bladder or bowel control.
When A Prickly Sensation Is No Longer Normal
Now that you have a clear vision of the reasons why you should not underestimate recurring episodes of numbness and pins and needles sensations, let’s look at when you should seek medical care.
Paresthesia can appear in two forms:
- Temporary: Also known as transient paresthesia, this is the most common form of pins and needles. It is commonly caused by temporary pressure on a nerve, does not last long, and can be resolved by shifting your position.
- Chronic: Chronic paresthesia can last for weeks or months, progress over time, or recur regularly. This is a symptom of an underlying condition that warrants medical attention.
Other signs that should prompt you to see a doctor include:
- The numbness is accompanied by persistent, dull pain.
- Paresthesia is interfering with your daily life.
You have other symptoms, including reduced range of motion, extreme sensitivity to touch, sleep problems, and disability.
Below, we’ll look at the tools used by your healthcare provider to diagnose the causes of your symptoms.
Diagnostic Procedures And Tests
As we have seen above, pins and needles are a symptom associated with more than one condition. Because of this, seeking an accurate diagnosis is the first step to finding the best line of treatment for your needs. Your healthcare provider will use a range of diagnostic tools to pinpoint the specific cause of your symptoms. These often include:
- Physical examination: A physical exam, which also may include a review of your symptoms and your medical history, is needed to determine the extent, location, and intensity of your paresthesia. Your doctor will also use manipulation and palpation to better understand which locations are affected by numbness, pain, and reduced range of motion.
- MRI or CT scans: Magnetic resonance imaging (MRI) and computerized tomography (CT) scans are used to obtain images of the inner aspect of your body. They can be utilized to identify abnormal tissues or mechanical problems that are compressing a nerve.
- Electromyography: This test is used to assess the ability of nerves to function properly and the quality of nerve signal transmission. It may help in identifying nerve or muscle dysfunction.
- Blood tests: Blood tests are prescribed when the suspected cause of your paresthesia is a medical condition such as diabetes.
Your doctor may also take biopsies (samples) of your skin to assess the count and function of nerves in the areas of your body where you have pins and needles.
Conventional Treatment Options
The line of treatment chosen to alleviate your symptoms and restore your musculoskeletal health largely depends on the underlying cause of paresthesia. Below, we’ll look at some of the most commonly prescribed therapies for chronic pins and needles.
Physical Therapy
Physical therapy may help restore physical function, especially when paresthesia derives from conditions like sciatica, weak core or back muscles, and inactivity.
If the pins and needles sensations are associated with reduced blood circulation, massage therapy and acupuncture may also help support circulation and relieve muscle tension, thus improving nerve function.
Physical therapy is more efficient when combined with necessary lifestyle changes (e.g. increased activity levels) and therapies that address the systemic inflammation at the root of conditions like diabetes, sciatica, and nerve damage.
Medications
Certain medications may help relieve the symptoms of a compressed or damaged nerve. These include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Painkillers
- Corticosteroid injections
- Capsaicin cream (Capsaicin is the active component in chili peppers.)
- Rubs, balms, and gels that can be applied topically
You may also be recommended specific pharmaceutical therapies to address the underlying condition that is causing the paresthesia. For example, if you have diabetes, you may be prescribed insulin and oral medications to manage your blood sugar levels.
Taking medications regularly to address chronic paresthesia can lead to severe side effects – including stomach ulcers and addiction – and let a more severe underlying condition go unaddressed. Be sure to find a treatment option that is both efficient and sustainable.
Surgery
Surgical interventions are prescribed when paresthesia begins to interfere with your daily life, cause disability, or do not respond to conservative treatments.
Depending on the cause of your symptoms, surgery may be used to:
- Enlarge the passageway that houses nerves to decompress them, such as in the case of carpal tunnel surgery
- Remove tissues that are pressing on the nerve, such as in the cause of discectomy when sciatica is caused by a herniated disc
- Correct mechanical issues, such as the ones deriving from a new or old injury.
Given the risks involved with surgery, this should only be considered as a last resort.
Neurofunctional Pain Management For Pain Caused By Pins And Needles
Treating pins and needles as a symptom isn’t just ineffective, but also dangerous. Relying on medications to alleviate your pain can let another, more severe disorder go undetected. Plus, you’ll expose yourself to unnecessary side effects that can further compromise your health!
However, often, paresthesia, nerve damage, and chronic disorders like diabetes can be traced back to a single cause: systemic inflammation. Neuragenex Neurofunctional Pain Management aims to address chronic pain and inflammation that is behind symptoms such as pins and needles. By kick-starting a positive feedback loop, this protocol can help you reduce your symptoms, boost your nervous system function, and lay the foundations of long-term health.
Learn about the pillars of Neuragenex Neurofunctional Pain Management below.
Electroanalgesia
Electroanalgesia is a pain management technique that uses high-pulse electrical current to ease pain, boost blood circulation, improve mobility, and induce...
IV Therapy
IV nutritional therapy, or intravenous therapy, involves administering vital nutrients directly to the bloodstream through an IV. This type of treatment bypasses the digestive system, allowing for maximum absorption and utilization of nutrients by the...
Lifestyle Counseling
Lifestyle counseling is an approach to managing chronic pain that involves identifying, assessing, and modifying lifestyle factors contributing to an individual's pain. For example, lifestyle factors such as nutrition, physical activity, stress, sleep quality...
Tackle Inflammation At Your Symptoms’ Roots
Chronic inflammation has been seen to be the single, most impactful cause of several chronic diseases affecting the population today, from diabetes to cardiovascular disorders, arthritis, and allergies. The entirely customizable approach aims to tackle chronic inflammation without medications or surgery so that you can restore your body’s function and health.
By tackling systemic inflammation and chronic pain at the root of disease, Neuragenex Neurofunctional Pain Management can help ease a range of symptoms and conditions, including the ones below.

Peripheral Neuropathy Pain Treatment
We offer a unique and leading-edge approach to treating the burning, tingling, throbbing pain that may be associated with peripheral neuropathy or nerve damage. We have helped 100’s of patients, just like you, reduce their pain fast and get back to living...

Fibromyalgia Pain Treatment
Fibromyalgia is a chronic disorder that causes several symptoms, including widespread pain, fatigue, and cognitive impairment. Our non-surgical and drug-free treatments can help reduce the chronic pain associated with fibromyalgia. Additionally, our holistic...
Get The Best Treatment For Paresthesia
Recurring episodes of pins and needles aren’t something that should be left unaddressed. This symptom can conceal severe disorders, including diabetes, multiple sclerosis, nerve damage, and sciatica.
Through our proprietaryNeuragenex Neurofunctional Pain Management protocol, can help you tackle the inflammation and chronic pain that is at the root of your paresthesia. So, you can regain your body’s function and sensation – without medications or invasive procedures.
Worried about surgeries and expensive treatments?




